Often people think rehab is about getting stronger and will do an old approach of taking a dysfunctional muscle and simply exercising it. The problem is rehabilitation isn't often about strength as much as it is about educating muscles. You can have the strongest muscles in the world but can get injuries if you dont teach them to fire properly or to work in the manner they should. The Popliteus is a great example of this concept as you never see people "working out" their Popliteus.
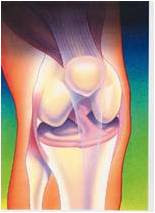
As mentioned previously the Popliteus is a muscle used mostly for kinesthetic awareness and stability in the knee. When an athlete pivots quickly or changes direction the Popliteus is put to work. When observing the picture below you can see how the muscle acts as a connection between the medial and lateral knee structures.
This means as the medial compartment experiences tension and the lateral side experiences compression the Popliteus receives this sensory feedback and stabilizes the knee. The opposite is also the same when the lateral side experiences tension and Medial experiences compression. This type of interaction occurs in the knee constently as an athlete brings the knee from flexion to extension and when performing pivoting moves.
So we need to rehabilitate it in a way that allows it to learn this function. However, how do you teach this function without putting stresses on the knee in an injured patient?

Exercises for the Popliteus
Exercises should consist of non-weight bearing and weight bearing exercises.
1. Using a resistant band attach one end to a stable service and the other around the forefoot of the affected leg. Using a wall for support begin the exercise with the affected leg unsupported at the patients side. From the start position begin flexing the knee and bringing the foot behind the stance leg as if attempting to touch your toe to your opposite hip. This creates flexion of the knee and internal rotation of the tibia. This motion will contract and activate the Popliteus. Now return to the starting position slowly to also train the Popliteus to contract eccentrically as well.
2. Stepping task - This exercise is used for progression and performed to challenge the Popliteus in a more functional manner. Using a small step up place one foot on the step allowing the knee to be maintained in a slightly flexed position. With the opposite leg off of the step bring yourself to a fencer type of stance.


Now while maintaining the supported knee in flexion begin different stepping manouvers. First going to 3 oclock back to start, 12 oclock and then 9 oclock. This exercise trains the Popliteus on how to prepare for cutting motions which will involve a forceful planting of the foot and manoeuvring in different directions.
The exercise can be further challenged by using verbal or visual cues to create a spongtanoise stepping action as apposed to the patient knowing where they will be going. Tossing a ball or using a racket can also make things more sports specific depending on the athlete. In addition, one can challenge the exercise by adding a blindfold to remove visual stimulus.
Once a patient displays proper technique in this exercise they may now progress to the same exercise above but using an unstable service.
3. Stepping Task Unstable Surface
4. The last exercise is done to train the Popliteus in a manner that challenges it to receive tension and then create a reflexive contraction. This involves a series of jumping task using pylons.
Standing alongside a pylon with one foot supported the patient jumps to the opposite side. The patient now has three options upon landing.
a) Land on the opposite leg they took off from allowing the Popliteus to be trained concentrically
b) Land on the same leg they took off from allowing the Popliteus to be used in a concentric to eccentric manner
c) Do option b followed by quickly jumping to the opposite side of the pylons allowing the Popliteus to be trained concentrically to eccentrically and then quickly concentrically again. This emulates a very quick stopping task or explosive take off manouver which man occur in multiple sports.
In summary, these are just a few quick exercises that can used in preseason training for athletes or any patient with knee problems. Dr. Wayne Button, BSc, DC
Nyland, J. (2005). Anatomy, Function, and Rehabilitation of the Popliteus Musculotendinous Complex Journal of Orthopaedic and Sports Physical Therapy DOI: 10.2519/jospt.2005.1414